
What are the symptoms of an ankle fracture?īecause a severe ankle sprain can feel the same as a fractured ankle, every ankle injury should be evaluated by a provider.Ĭommon symptoms for a fractured ankle include: Multiple ligaments help make the ankle joint stable. Syndesmosis joint - the joint between the tibia and fibula, which is held together by ligaments.Ankle joint - where the tibia, fibula, and talus meet.

Two joints are involved in ankle fractures: For example, a fracture at the end of the fibula is called a lateral malleolus fracture, or if both the tibia and fibula are fractured, it is called a bimalleolar fracture. Providers classify ankle fractures according to the area of bone that is broken. Posterior malleolus - back part of the tibia.Medial malleolus - inside part of the tibia.The tibia and fibula have specific parts that make up the ankle: Talus - a small bone that sits between the heel bone (calcaneus) and the tibia and fibula.During the past 30 to 40 years, doctors have noted an increase in the number and severity of fractured ankles, due in part to an active, older population of baby boomers. The ligaments of the ankle hold the ankle bones and joint in position.įractured ankles affect people of all ages. Simply put, the more bones that are broken the more unstable the ankle becomes. We offer diagnosis and treatment in over 70 specialties and subspecialties, as well as programs, services, and support to help you stay well throughout your lifetime.Ī fractured ankle (broken ankle) means that one or more of the bones that make up the ankle joint are broken.Īn ankle fracture can range from a simple break in one bone, which may not stop you from walking, to several fractures, which forces your ankle out of place and may require that you not put weight on it for a few months.
Talus fracture treatment professional#
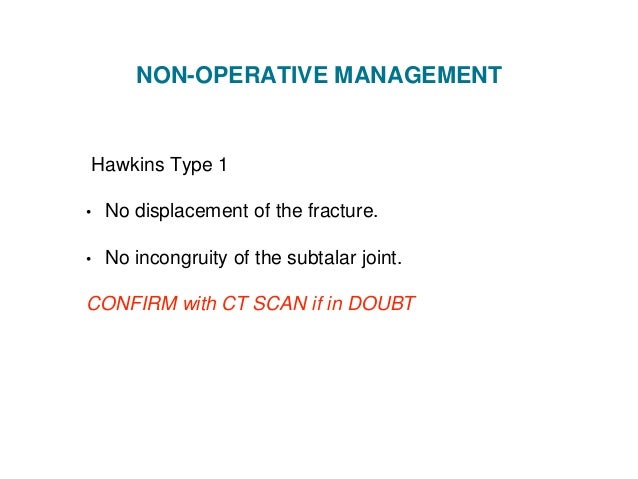
Talus arthritis arthroscopy fracture fractures malunion subtalar joint talar body talus complications talus management.BMC physicians are leaders in their fields with the most advanced medical technology at their fingertips and working alongside a highly skilled nursing and professional staff. The various complications are avascular necrosis, malunion, infections, late osteoarthritis, and ankylosis of subtalar joint. Clinical outcomes depend on the severity of the initial injury and the quality of reduction and internal fixation. Sometimes, a dual approach with a malleolar osteotomy is necessary for articular restoration. Surgery is indicated in most of the cases, and different approaches have been described. Splinting, followed by short leg casting for 6 weeks until fracture union should be undertaken. Indications for nonoperative management are seldom indicated and are few as in nonambulatory patients, or in with multiple comorbidities who are not able to tolerate surgery. Optimal treatment relies on an accurate understanding of the injury and the goals of treatment are the restoration of articular surface and axial alignment. Differentiating talar neck from body fractures is important. The initial evaluation should be done with foot, and ankle radiographs and computed tomography is often done to analyze the extent of the fracture, displacement, intraarticular extension, comminution, and associated fractures.

Associated neurovascular injury of the foot should be carefully examined. Clinically, talar body fractures present with soft tissue swelling, hematoma, deformity, and restriction of motion. Great care is necessary for diagnosing and treating these injuries. Axial compression with supination or pronation is the common mechanism of injury. They occur as a result of high-velocity trauma and are therefore associated with considerable soft tissue damage. The relative infrequency of this injury limits the number of studies available to guide treatment. The integrity of the talus is essential for the normal function of the ankle, subtalar, and midtarsal joints. Fractures of talar body are uncommon injuries often associated with fractures of other long bones and in polytraumatized patients.


 0 kommentar(er)
0 kommentar(er)
